Transoral robotic surgery for the management of laryngeal and hypopharyngeal cancers: A Review
Nauar Knightly UCD School of Medicine and Medical Science, University College Dublin, Belfield, Dublin 4, Ireland
ABSTRACT
Transoral robotic surgery (TORS) is being employed more frequently to perform tissue sparing surgery for the management of cancers of the aerodigestive tract. The uptake of TORS can be attributed to encouraging results of functional and aesthetic outcomes when compared to open surgery, and the widely practiced transoral laser microsurgery (TLM). There is also a trend towards performing more technically challenging surgeries using advancements in technology and robotics in order to preserve quality of life (QOL), whilst maintaining favourable outcomes and overall survival. The aim of this review was to assess the functional and oncologic outcomes of the evolving TORS. A ScienceDirect search was carried out to find studies reporting the functional and survival outcomes using TORS for the treatment of laryngeal and hypopharyngeal cancers. QOL postoperatively was also considered. One hundred and sixty-six results were displayed by ScienceDirect. In total 11 papers were identified providing information regarding outcomes associated with TORS.
TORS offers no improvement in survival for the management of laryngeal and hypopharyngeal cancers when compared to laser microsurgery or open surgery. However, TORS offers improved functional and aesthetic outcomes with faster recovery times and reduced postoperative pain when compared to open surgery. Although the functional outcomes are similar to TLM, it does not have the technical drawbacks of TLM and has greater future potential, utilising its sophisticated high definition 3D visualisation, tremor free handling and malleable controls.
Article
Introduction
Cancers of the oropharynx, hypopharynx and larynx are intimately related to smoking, alcohol and HPV infection. The incidence of these cancers is rising in the developing world due to the recent surge in HPV infection [1, 2]. Head and neck surgery was historically aggressive with large amounts of tissue excision and dissection, resulting in collateral damage to the surrounding structures. The focus is on improved QOL, functional preservation and use of minimally invasive techniques, with emphasis on minimal tissue dissection to achieve these goals [3, 4, 5, 6, 7]. Current challenges are adequate illumination and visualisation, especially in locations such as the piriform sinus [8, 9, 10, 11]. The benefits offered by robotics are improved visualisation, elimination of physiological tremor and untiring actions in difficult positions facilitated by EndoWrist [7, 8, 9]. The robotic assistance allows for multi-planar dissection. The system consists of the surgeon console, patient side robotic cart and a high definition 3D vision system [8, 9, 10, 11].
“TORS has surpassed what is offered by radical open approaches in terms of operation times, reduction in overall morbidity and faster recovery times”
TORS has surpassed what is offered by radical open approaches in terms of operation times, reduction in overall morbidity and faster recovery times [4, 8, 9]. When compared to TLM the results are more modest. The limitations of TLM include the distance between the surgeon and operating field as well as restriction to single handed use for tissue manipulation, while using the other to operate the laser [1, 3]. Thus far studies reporting the functional outcome and benefits of TORS consist of small cohorts and carefully selected patients who undergo comprehensive assessment prior to being considered for the surgery. Today TORS has been adopted widely across North America and is making progress establishing itself across European centres.
Methods
A literature search of ScienceDirect was performed on all original articles describing transoral robotic surgery. This database was chosen because it provided results for numerous studies on the subject and unrestricted access to all the relevant literature. Only articles written in English were considered. Review articles were read for background knowledge but were not included in the results of this review. Search terms used were, “transoral robotic surgery on pharynx”, “transoral surgery for laryngeal cancer”, “robotic surgery for neck cancers”, “TORS for hypopharyngeal cancer”, “robotic surgery for laryngeal cancers” and “robotic surgery for hypopharyngeal cancer”.
Inclusion criteria:
Studies that examined the outcomes of TORS for hypopharyngeal cancers
Literature comparing the outcomes of TORS to TLM or open surgery
Subjects 18 years or older
Malignant lesions
Original research
Results
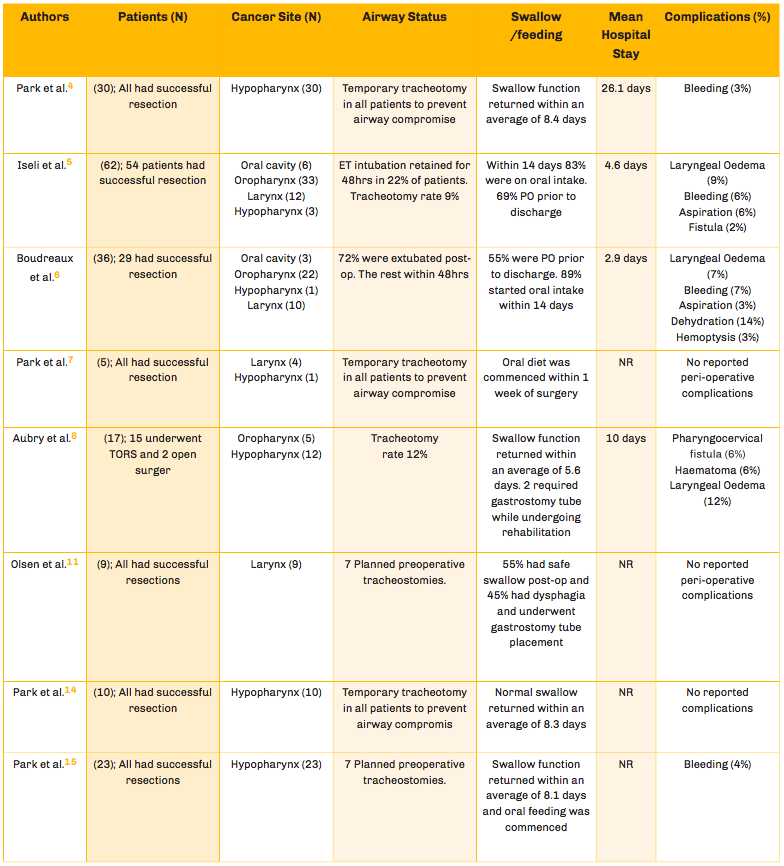
There were a total of 166 results. Irrelevant results were studies which focused on non-surgical treatments of head and neck cancers. They were excluded based upon their abstract description. Review papers were also filtered out alongside correspondence articles. The eight papers which published results on the transoral robotic approach and compared them to results from more conventional methods of surgery (open surgery and TLM) are outlined in (Table 1).
Patient Demographics
The gender, mean age and follow up time were extrapolated from the research papers. The mean age of patients across the studies listed in (Table 1) was 63.1 years. The patient cohorts consisted predominantly of male patients, which made up 80% of the patients across the studies. The follow-up times reported varied significantly, ranging between 3-36 months with some studies not reporting any follow-up.
Treatment
Patients who underwent TORS were assessed prior to surgery with full physical examination, CT, PET-CT and panendoscopy with biopsy to confirm the diagnosis. Patients were excluded if the disease was deemed to be too advanced for surgical intervention or too invasive to vital surrounding structures. When the tumours were resected, peripheries of the tissue were checked for clear margins via frozen section in the pathology department. Positive margins were re-excised until clear borders were achieved. Following this neck dissection was performed in most circumstances.
Technical and Oncologic Outcomes
When operating times are considered, the robotic system is overall twice as efficient as the open approach, even when the robot set-up time is considered [4] which is a statistically significant difference (p < 0.001). TORS for the management of laryngeal and hypopharyngeal cancer is safe, versatile and oncologically impressive, with studies reporting their entire cohort disease free at 6 & 12 months8,14 and other literature data describing an 83-89% overall survival at 3-years [4, 15]. Research papers with long term follow-ups (18-22 months) have shown a mortality ranging from 9-14% [4, 15]. There are some impressive results from Olsen et al. [11] which showed complete disease control in 77% of the patients (at 24 months), most of who had stage II-IVa disease. When compared to radical surgery, TORS has a slightly superior outcome (5-8%) [4] in terms of 3-year disease free survival and overall survival but the difference is not statistically significant. It should be noted that the majority of these patients who underwent TORS also had some form of adjuvant therapy whether chemotherapy, radiotherapy or both depending on the stage of the disease. Lastly, in-spite of the fact that overall survival between open surgery and TORS is not statistically significant, what must also be considered is recovery, long term functional outcomes and QOL.
Functional Outcomes
Tracheotomy was performed in a few studies. This was to prevent airway compromise secondary to laryngeal oedema or a haematoma [4, 7, 14, 15]. Laryngeal oedema was a documented post-op complication in a few cases where tracheotomy was not routinely performed as a preventative measure. In such cases, emergency intervention was necessary to maintain a patent airway [3, 5, 6, 8]. Intraoperative corticosteroids injections were also employed as a different technique used to minimise the risk of laryngeal oedema.8
A basic outline of the swallowing and feeding outcomes can be seen in (Table 1). Patients who underwent open surgery reported post-operative dysphagia and odynophagia [4, 14].
Bordeux et al noted that 30% of their patients were nasogastric tube (NGT) dependent postoperatively due to severe dysphagia [6]. Olsen et al reported NGT placement in patients who had significant dysphagia and lacked a safe swallow [11]. The average time patients spent on NGT feeding post TORS was approximately 8 days [4, 5, 6, 7]. In comparison, radical open surgery required NGT feeding for at least 11 days, with the average time of 20.6 days [4]. The same study [4] showed that three times as many patients who had undergone open surgery ended up on long term PEG feeding in contrast to the TORS group. Therefore swallowing function outcome is superior in the TORS group compared to the open surgery cohort (p <0.001).
Problems with phonation are frequently overlooked and under-reported in the literature with particular studies failing to mention it in their results [5, 6, 8]. Olsen et al. measured speech outcome using 3 parameters: phonation, resonance and articulation. Speech was possible without long term issues in particular cases [7, 14]. Park et al documented detailed reports of the voice outcome in his 3-year follow up study [15]. The assessment of speech was evaluated through acoustic waveform analysis which showed that frequency variation and jitter occurred in patients after piriform sinus resection because the ipsilateral vocal cord dexterity was affected from the resection.
Quality of Life
This was assessed using the University of Washington Quality of Life Scale, after a minimum of 6 months following surgery [4]. When TORS was compared to open surgery, it surpassed it terms of chronic pain (p = 0.013), cosmesis (p = 0.005), physical activity (p = 0.009), speech (p < 0.001), swallow (p = 0.003) and anxiety (p = 0.004). In addition, a better overall health related outcome was achieved in the TORS cohort [4].
QOL does decline post op from baseline in terms of speech, swallowing and cosmesis. This is most notably seen in patients who received adjuvant radiotherapy. Fortunately, QOL continuously improves with time and at 12 months follow up there was no statistically significant difference in the QOL from baseline [3].
Complications
Threats to the airway are the main postoperative concern. Laryngeal oedema is the most commonly reported complication in many of the studies; it necessitates emergency intervention and is a cause of morbidity. There was only 1 reported case of laryngeal haematoma compromising the patency of the airway and necessitating emergency surgical drainage. Park et al. routinely perform tracheotomies to avoid these complications involving the airway, which have a incidence of <10% based on the literature data reviewed (Table 1). Haemorrhage is the second most common issue encountered postoperatively. Bleeding can occur acutely post-op or chronically months after the initial procedure.
Table 1
Discussion
TORS has impressive oncologic outcomes with overall survival of up to 89% at 3-years [15]. Hypopharyngeal cancer has the worst prognosis of the aerodigestive cancers [4, 7, 15]. The survival benefit of TORS is equal to open surgery and primary radiotherapy, but it is superior in terms of functional outcome, reduced post-op pain and better quality of life [3, 4, 6, 7, 8].
Patients who underwent TORS in the studies reviewed were meticulously selected, received physical examinations, CT imaging, PET-CT and panendoscopy to assess the full extent of the disease prior to selection for TORS. Resectable tumors were selected for these studies, and some authors reported up to 100% success rate [10]. Inherent selection bias for lower stage cancers was noted due to the experimental design of the studies and the cautious patient selection [4]. Accessibility is still an issue concerning certain anatomical sites, but site exposure can be maximised with specific setups, tools and patient positioning. This facilitates access to more challenging anatomical locations such as the piriform sinus [10].
Many of the research articles are based on small patient cohorts, making it difficult to draw confident conclusions from the small sample size.
Long-term NGT dependence was examined by Bordeux and Dziegielewski [3, 6]. Dependence was associated with more advanced disease (pT3/pT4), advanced age and a lower MDADI score [6]. Patients with pT3/pT4 neoplasms are 27 times more likely to remain on long term NGT.3 TLM became the new standard of treatment after demonstrating better functional outcomes compared to open surgery especially in speech and swallowing [16a-c]. However TLM has technical limitations, mainly the issue of limited mobility and line of sight limitations. This means that resection is only possible in one direction. TORS has the capacity to overcome the technical limitations of TLM, facilitating superior visualisation, with the use of a movable camera with three-dimensional views, magnification and high-definition video output [14].
Limitations of Robotic Surgery
The potential technical capabilities of robotic surgery are alluring, often obscuring the limitations of this new technology. The cost of the DaVinci robot is €1.7 million with an annual maintenance cost of up to €140,000. Despite the costs, this investment does not improve survival when compared to the accepted standard of transoral laser microsurgery, making it a luxury for many clinical centres in Europe.
The cost of the DaVinci robot is €1.7 million with an annual maintenance cost of up to €140,000
A notable limitation of the technology is the requirement of acute angles of approach when using the multiple robotic arms through the oral opening. This limitation is worsened by interference between the multiple robotic arms, which requires manual repositioning for conflict resolution. This is especially problematic when operating on deeper structures of the aerodigestive tract such as the deeper recesses of the piriform sinus.
conclusion
TORS has achieved competitive outcomes when compared to TLM and radical open surgery and is quickly evolving in its use for neoplasms of the head and neck. It has potential to become the new standard of care following encouraging results in terms of functional outcome and QOL. Indication for its use is growing as surgeons build experience and new techniques are applied. In conclusion, the evidence suggests that TORS is a valid, safe and minimally invasive procedure which should be considered when managing laryngeal and hypopharyngeal cancers.
References
Yeh, D. H., S. Tam, K. Fung, et al. 'Transoral Robotic Surgery Vs. Radiotherapy for Management of Oropharyngeal Squamous Cell Carcinoma - A Systematic Review of the Literature', European Journal of Surgical Oncology : The Journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology. 2015; 41: 1603-1614.
Wojciech K. Mydlarz, Jason Y.K. Chan, Jeremy D. Richmon. The role of surgery for HPV-associated head and neck cancer. Oral Oncology. 2015; 51: 305-313.
Dziegielewski PT, Teknos TN, Durmus K, et al. Transoral Robotic Surgery for Oropharyngeal Cancer: Long-term Quality of Life and Functional Outcomes. JAMA Otolaryngology–Head & Neck Surgery. 2013; 139: 1099-1108.
Park YM, Byeon HK, Chung HP, Choi EC, Kim SH. Comparison study of transoral robotic surgery and radical open surgery for hypopharyngeal cancer. Acta Oto-Laryngologica. 2013; 133: 641-648.
Iseli A, Kulbersh BD, Iseli CE, Carroll WR, Rosenthal EL, Magnuson JS. Functional outcomes after transoral robotic surgery for head and neck cancer. Otolaryngology - Head and Neck Surgery. 2009; 141: 166-171.
Boudreaux BA, Rosenthal EL, Magnuson JS, et al. Robot-Assisted Surgery for Upper Aerodigestive Tract Neoplasms. Archives of Otolaryngology–Head & Neck Surgery. 2009; 135: 397-401.
Park YM, Lee WJ, Lee JG, Lee WS, Choi EC, Chung SM, Kim SH. Transoral Robotic Surgery (TORS) in Laryngeal and Hypopharyngeal Cancer. Journal of Laparoendoscopic & Advanced Surgical Techniques. 2009; 19: 361-368.
Aubry K, Yachine M, Perez AF, Vivent M, Lerat J, Scomparin A, Bessède JP. Transoral robotic surgery for head and neck cancer: A series of 17 cases. European Annals of Otorhinolaryngology, Head and Neck Diseases. 2011; 128: 290-296.
Garg A, Dwivedi RC, Sayed S, et al. Robotic surgery in head and neck cancer: A review. Oral Oncology. 2010; 46: 571-576.
De Virgilio A, Park YM, Kim WS, Baek SJ, Kim S. How to optimize laryngeal and hypopharyngeal exposure in transoral robotic surgery. Auris, nasus, larynx. 2013;40:312-319.
Olsen SM, Moore EJ, Koch CA, Price DL, Kasperbauer JL, Olsen KD. Transoral robotic surgery for supraglottic squamous cell carcinoma. American Journal of Otolaryngology. 2012; 33: 379-384.
A) Canis M, Ihler F, Martin A, Wolff HA, Matthias C, Steiner W. Organ preservation in T4a laryngeal cancer: is transoral laser microsurgery an option? Eur Arch Otorhinolaryngol. 2013; 270: 2719–27.
B) Canis M, Ihler F, Martin A, Wolff HA, Matthias C, Steiner W. Results of 226 patients with T3 laryngeal carcinoma after treatment with transoral laser microsurgery. Head Neck. 2013.
C) Steiner W, Vogt P, Ambrosch P, Kron M. Transoral carbon dioxide laser microsurgery for recurrent glottis carcinoma after radiotherapy. Head Neck. 2004; 26: 477–84.
Weinstein GS, O’Malley BW, Hockstein NG. Transoral robotic surgery: supraglottic laryngectomy in canine model. Laryngoscope. 2005; 115: 1315-19.
Park YM, Kim WS, Byeon HK, De Virgilio A, Jung JS, Kim SH. Feasibility of transoral robotic hypopharyngectomy for early-stage hypopharyngeal carcinoma. Oral Oncology. 2010; 46: 597-602.
Park YM, Kim WS, Byeon HK, De Virgilio A, Jung JS, Kim SH. Transoral robotic surgery for hypopharyngeal squamous cell carcinoma: 3-Year oncologic and functional analysis. Oral Oncology. 2012; 48: 560-566.
Esteban F, Menoyo A, Abrante A. Critical Analysis of Robotic Surgery for Laryngeal Tumours. Acta Otorrinolaringologica (English Edition). 2014; 65: 365-372.
Mandapathil M, Teymoortash A, Güldner C, Wiegand S, Mutters R, Werner JA. Establishing a transoral robotic surgery program in an academic hospital in Germany. Acta Oto-Laryngologica. 2014; 134: 661-665.